2/2/17
We do not diagnose disease or recommend a dietary supplement for the treatment of disease. You should share this information with your physician who can determine what nutrition, disease and injury treatment regimen is best for you. You can search this site or the web for topics of interest that I may have written (use Dr Simone and topic).
“We provide truthful information without emotion or influence from the medical establishment, pharmaceutical industry, national organizations, special interest groups or government agencies.” Charles B Simone, M.MS., M.D.
OFTEN NEGLECTED AND UNDIAGNOSED CAUSE OF WOMEN’S CHEST PAIN – CORONARY MICROVASCULAR ANGINA (SYNDROME X)
Lawrenceville, NJ (Dr Simone) – Microvascular angina affects mainly women, and occurs predominately in postmenopausal women. These women are often neglected and diagnosed as having “non-cardiac” chest pain, and are sometimes given no treatment. However, microvascular angina has important implications because these women have a 1.5 fold increase (150%) in cardiac muscle damage or death compared to those without evidence of heart ischemia. Also, more that 40% are readmitted to the hospital for chest pain, and 30% undergo repeat coronary angiography. They also have a worse quality of life.
The symptom “chest pain” has many causes. Coronary angiography can determine if the coronary arteries have obstructions (plaque) that cause chest pain as a result of low oxygen delivery to the heart (ischemia). But small microvessels cannot be seen using angiography and therefore these microvessels must be evaluated differently. Overall 10% to 25% of women with acute coronary syndrome have a “normal” coronary angiography. In fact, no obstructions are seen and a normal diagnosis is made five times more frequently in women than in men. The walls of these microvessels are damaged or diseased leading to spasms and reduction of blood flow. Even though people may have the same risk factors for heart disease, some of them develop microvascular disease and some people develop large vessel coronary artery disease. The usual treatments for coronary microvascular angina are not totally effective.
Microvascular angina (small vessel disease), also known as Syndrome X, is characterized by:
– Symptoms: angina (chest pain) with exertion or during stress without physical exertion, shortness of breath, sweating, nausea, dizziness, pain in left arm, jaw, neck, back or abdomen associated with chest pain, fatigue, lack of energy.
– Abnormal stress test that indicates cardiac ischemia
– Appearance of normal or near normal coronary arteries on angiography
(see below)
– Absence of other specific cardiac disease, such as valvular disease, Prinzmetal angina, etc.
As a student I worked with a cardiologist, Barry Ultan M.D., with patients who had chest pain, shortness of breath, leg ache, and were diagnosed as having miniscule pulmonary emboli due to a smoldering thrombophlebitis (See ABSTRACT BELOW). These patients today might be diagnosed as having microvascular angina, or Syndrome X. I thought their chest pain was related to clinical episodes of hypoglycemia. So I looked at their glucose levels over a six hour period of time and “Redefined Reactive Hypoglycemia showing that the speed with which glucose fell was more important than an arbitrary absolute level. The results suggested that more epinephrine is released for those who have a rapid and steep fall in glucose in order to push up and normalize the blood glucose as quickly as possible. This epinephrine “kick” might predispose to smoldering thrombophlebitis and vascular disease.”
Now, decades later, this hypothesis has since been confirmed by other researchers showing that hypoglycemia does indeed cause increased clot formation and increased inflammation, with effects lasting up to 7 days after a hypoglycemic event (Chow et al. Lancet. Feb 26, 2014. pg 35).
Microvascular Angina affects:
– 30% of stable angina patients with non-obstructive coronary arteries.
– 20% of women with acute coronary syndrome
– 30% of women presenting with unstable angina – a precursor to myocardial infarction
– 20% of women presenting with myocardial infarction
Diagnosis
Stress Test – with or without nuclear scanning
Coronary Angiogram
Endothelial dysfunction test. When your doctor can’t find blockages in your main arteries, you might need this test. The endothelium is a thin layer of cells that line the interior surface of blood vessels. The endothelium secretes substances that regulate vascular tone, platelet activity, coagulation, and influences vascular inflammation and cell migration. The endothelial dysfunction test measures how well the endothelial cells stretch and expand. Endothelial dysfunction is characterized by impaired nitric oxide (NO) bioavailability, increased nitric oxide (NO) breakdown by reactive oxygen species, or both. Nitric Oxide is needed for normal blood vessel dilation.
Through a catheter in one of your coronary arteries, a medication (acetylcholine) is injected that increases the release of Nitric Oxide causing the small vessels in your heart to open. Then the blood flow through those vessels is measured. This invasive test is an accurate way to detect small vessel disease.
Treatment for Microvascular Angina
The main goal of treatment is to control symptoms of chest pain. The medications used for classical obstructive coronary artery disease are the same that are used for microvascular angina but are somewhat less effective. In fact, there are no large randomized studies that investigated the effect of the classical anti-anginal drugs on the improvement of symptoms and prognosis of patients with microvascular angina.
Classical Anti-Anginal Drugs
-
Nitroglycerin is not recommended for patients with microvascular angina because they have minimal effects on small microvessels.
-
Beta Blockers, recommended as first line treatment, slow your heart rate and decrease your blood pressure. Third generation beta-blockers like carvedilol stimulate the release of nitric oxide from the microvascular endothelium helping to dilate these small vessels.
-
Calcium Channel Blockers relax the muscles around your coronary blood vessels, allows them to open, thus increasing blood flow to your heart. They also lower high blood pressure (eg. verapamil, diltiazem). They are recommended if beta-blockers do not help or are not tolerated.
-
Angiotensin-converting Enzyme (ACE) inhibitors open your blood vessels and lower your blood pressure (eg. lisinopril).
-
Angiotensin II Receptor Blockers (ARBs) relax your blood vessels, lowers your blood pressure, and makes it easier for your heart to pump blood (eg. losartan, valsartan).
-
Agent that alters sodium and calcium levels ease chest pain without reducing heart rate or blood pressure (eg. ranolazine)
-
Phosphodiesterase-5 inhibitor is a drug under clinical investigation (Clinical Trials.gov: NCT01769482) that allows more Nitric Oxide to be available. This is the same class of drugs used for Erectile Dysfunction and Pulmonary Hypertension.
-
Aspirin decreases inflammation and prevents blood clots. Read my Report: ASPIRIN – WHAT DOSE, WHAT FORM, WHEN TO TAKE IT, BENEFIT
-
Statins have properties of antioxidants, anti-inflammatories, and can lower cholesterol.
-
L-Arginine, an over-the-counter amino acid, increases Nitric Oxide that relaxes your blood vessels.
Dr Simone’s Recommendations:
1) Follow Dr Simone’s Ten Point Plan ( http://drsimone.com/tenpoint.htm ) to decrease your risk of developing heart disease and to decrease progression of heart disease if you have it. Take nutrients as outlined.
2) Consult with a cardiologist who treats Microvascular Angina (Syndrome X) to make a diagnosis and institute treatment.
3) L-Arginine 1000 mg twice a day with food if you have Microvascular Angina, in addition to the prescriptions medicines.
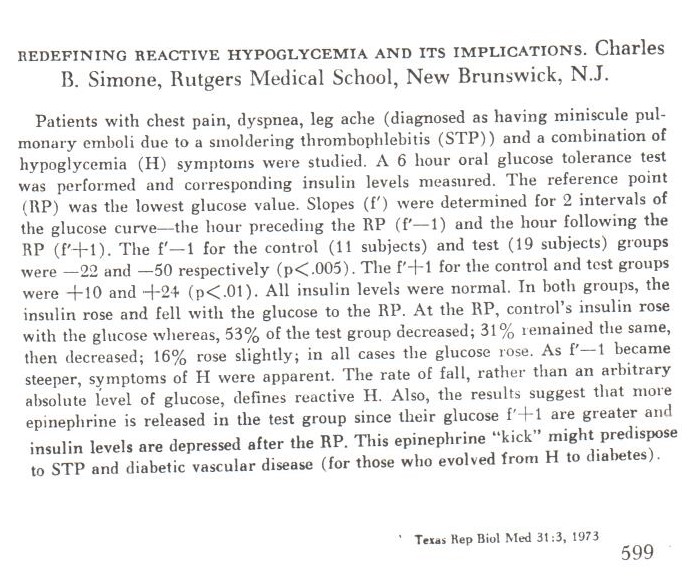
Redefining Reactive Hypogylcemia
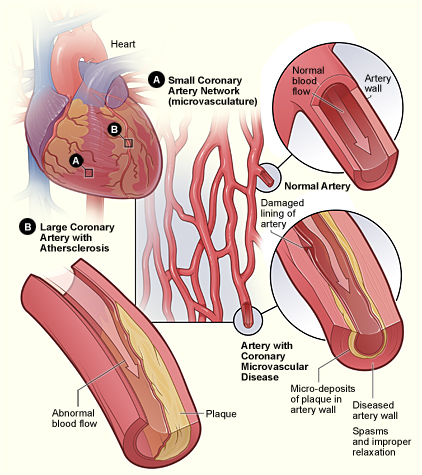
Microvascular Disease
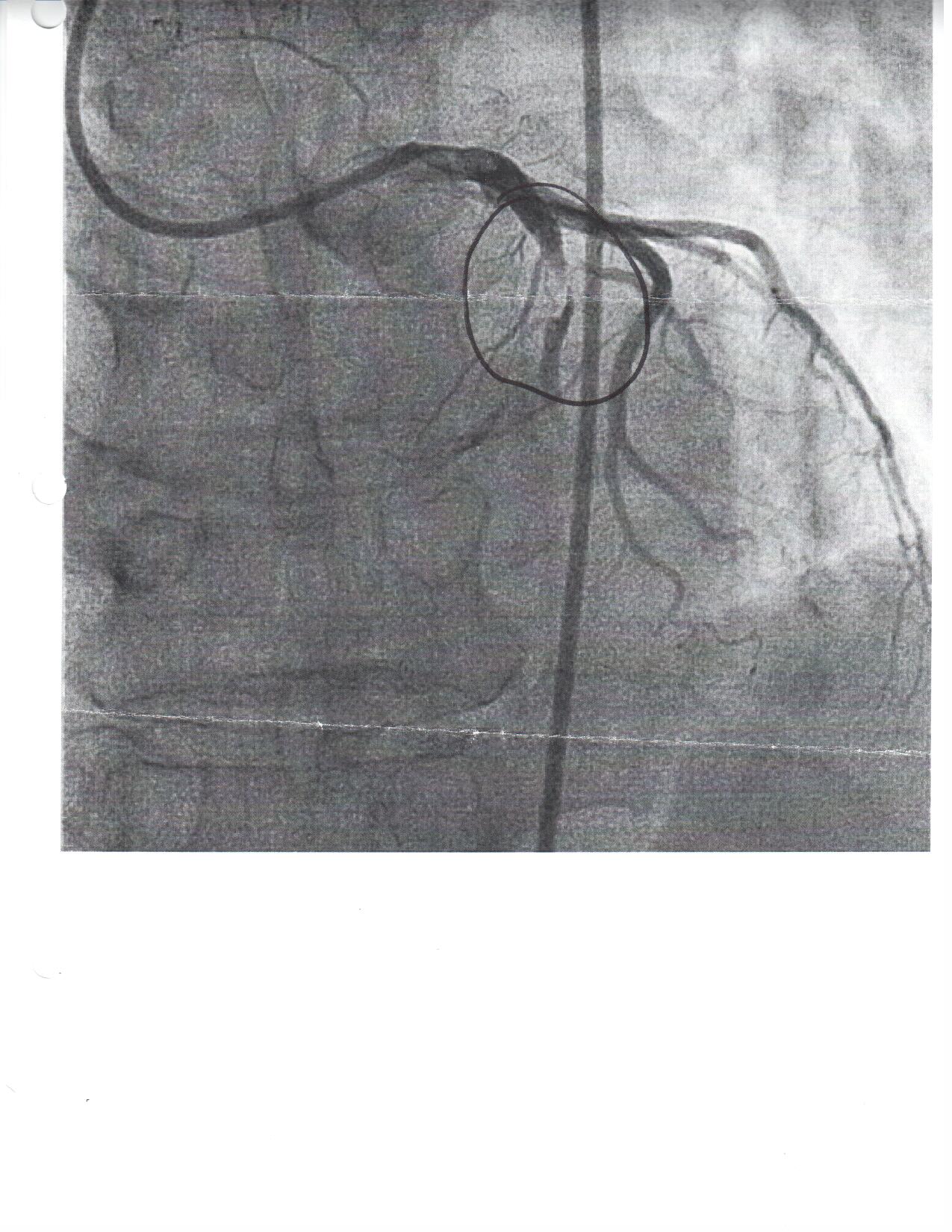
Non-microvascular Obstruction Caused by Clot, Plaque, etc.
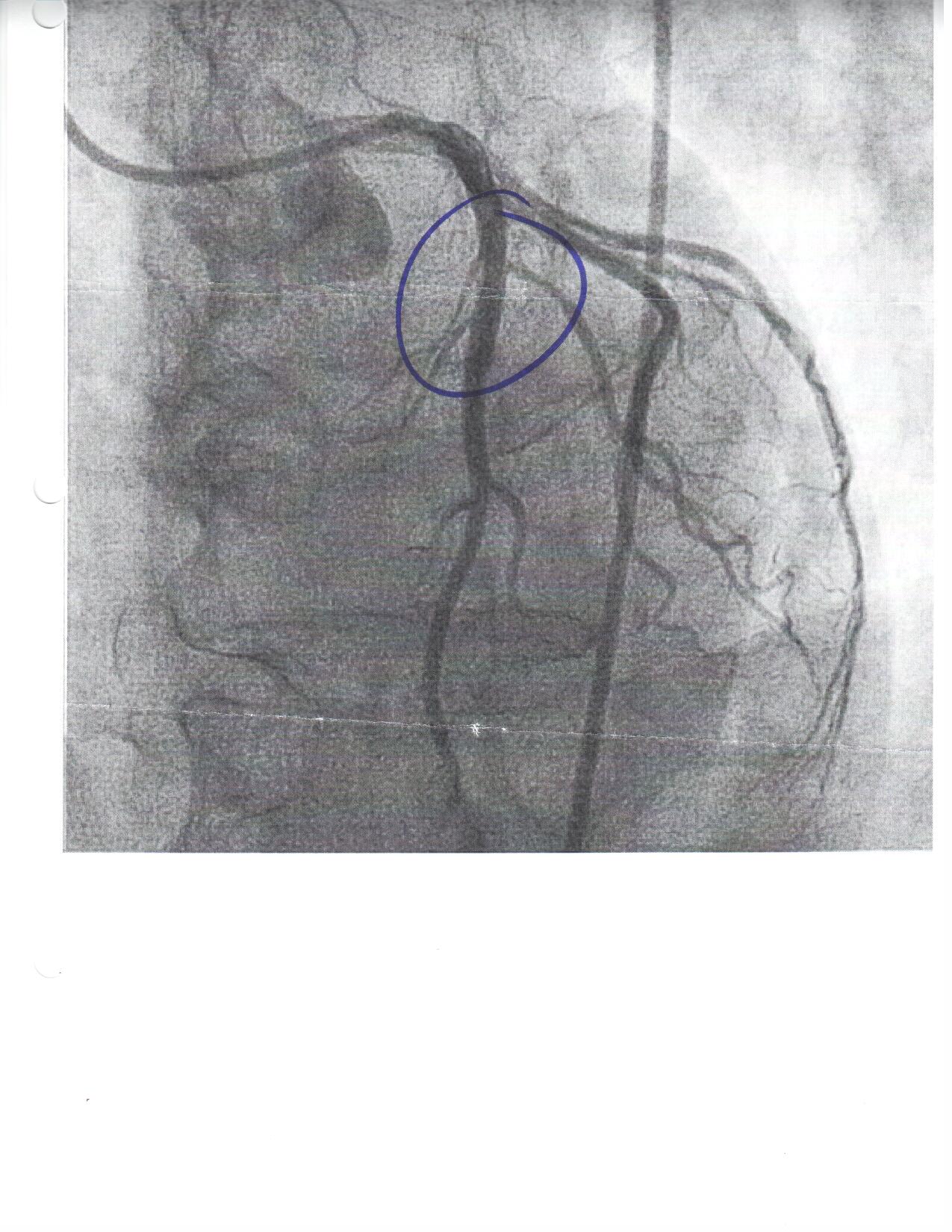
Stent Placed to Open Non-microvascular Obstruction